Pediatric cancer relapse prediction has emerged as a critical development in the ongoing battle against childhood cancers, particularly for conditions like brain tumors or gliomas. Recent advancements in AI cancer prediction have significantly improved the ability to anticipate relapse risk, outperforming traditional methods and providing hope for better patient outcomes. By leveraging cutting-edge techniques such as temporal learning AI, researchers are able to analyze a series of brain tumor imaging scans over time, identifying subtle changes that may indicate a higher risk of recurrence. This proactive approach not only alleviates the stress of frequent imaging but also helps to tailor treatment plans that could enhance survival rates in pediatric oncology. As we continue to explore innovative methods in cancer care, the integration of predictive AI technologies is revolutionizing how we manage and monitor pediatric cancer patients, ultimately aiming for more personalized and effective interventions.
The prediction of relapse in children diagnosed with cancer represents a pivotal area of research that seeks to enhance treatment protocols. Utilizing advanced algorithmic strategies, including longitudinal imaging analyses, healthcare professionals are increasingly capable of determining recurrence likelihood for various cancer types, specifically in pediatric populations. Techniques like temporal learning facilitate a comprehensive review of multiple imaging studies, which is essential in understanding conditions such as glioma recurrence. This innovative paradigm not only seeks to improve outcomes but also aims to ease the burden on families navigating the complexities of pediatric oncology. As studies continue to unfold, it is clear that embracing AI’s potential will redefine the future of cancer treatment and monitoring.
Advancements in AI for Pediatric Cancer Prediction
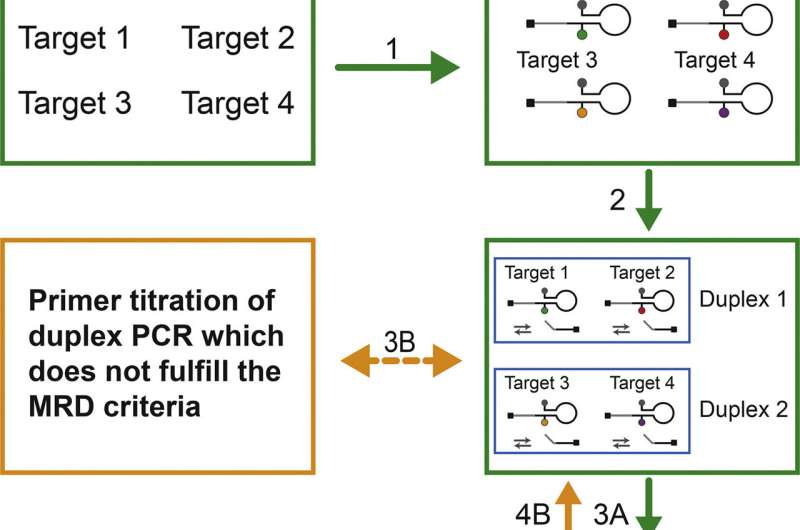
The integration of artificial intelligence (AI) in predicting pediatric cancer relapse heralds a transformative shift in pediatric oncology. Traditional methods of assessing cancer recurrence largely rely on linear analyses of individual magnetic resonance imaging (MRI) scans, which can lead to uncertainty and inefficiencies. The recent study highlights a novel AI tool that leverages temporal learning AI techniques, enabling the model to analyze multiple scans taken over time. This approach significantly improves the accuracy of predicting relapse risk in children with gliomas, a type of brain tumor that, while treatable, can be prone to recurrence.
AI cancer prediction models, particularly those employing temporal learning, offer a more nuanced understanding of tumor dynamics and growth patterns. By utilizing sequential imaging data, healthcare providers can identify subtle changes that may indicate an imminent relapse, a capability that traditional methods struggle to achieve. As researchers continue to refine these models, they anticipate a future where AI not only aids in diagnosing initial tumors but also plays a critical role in monitoring post-treatment recovery and predicting potential recurrences.
The Role of Temporal Learning in Cancer Imaging
Temporal learning is an innovative approach that sets itself apart from traditional single-scan evaluation methods. In this context, it enables AI systems to assess serial images of patients more holistically, by understanding the evolution of their brain tumors over time. This continuous-learning paradigm is crucial, particularly in pediatric oncology, where patients undergo routine imaging for years after treatment. The ability to gauge tumor behavior based on trends rather than isolated events provides a much greater predictive power.
The findings from the recent study reveal that the temporal learning AI model achieved impressive accuracy rates between 75-89% for predicting cases of glioma recurrence one year post-treatment. This accuracy starkly contrasts with standard predictive measures that hover around just 50%, emphasizing the potential of temporal learning AI in enhancing healthcare outcomes. As more research validates these initial results, there is significant optimism that this approach could redefine how healthcare professionals manage and monitor pediatric patients with high-risk brain tumors.
Impact of AI on Family Stress in Pediatric Cancer Care
The emotional toll of pediatric cancer treatment can be profound not only on the patients but also on their families. Frequent MRIs and the uncertainty surrounding potential relapses often lead to significant anxiety and stress. By employing advanced AI tools that reliably predict relapse risks, healthcare teams can alleviate some of this burden. An optimized prediction model helps streamline follow-up protocols, meaning that low-risk patients may require less frequent imaging, thus reducing the overall strain on families during recovery.
Healthcare professionals recognize that better relapse prediction methods can lead to more personalized patient care plans. For example, families of low-risk patients can be assured with a degree of confidence that fewer MRIs will be necessary, freeing them from constant worry about their child’s health status. Moreover, a definitive risk assessment allows high-risk patients to be preemptively treated with targeted therapies, potentially leading to better outcomes. As AI continues to evolve in this field, its role in not just patient health, but also in improving the quality of life for families, is becoming increasingly evident.
Exploring the Challenges of AI in Pediatric Oncology
While the potential advantages of AI in predicting pediatric cancer relapse are significant, the transition from research findings to clinical application poses several challenges. First, the need for extensive validation across diverse patient populations is paramount to ensure that the AI tools are reliable and applicable in various clinical settings. Current studies have focused primarily on specific institutions, meaning the generalizability of the findings is still in question and requires broader datasets, including variations in demographics and tumor characteristics.
Another challenge lies in the integration of these AI systems into existing healthcare frameworks, which may already be burdened with protocols and technological constraints. Healthcare providers will need comprehensive training to effectively utilize AI tools in their practice. Moreover, considerations surrounding data privacy and the ethical use of AI in medicine must be addressed to gain trust and acceptance among clinicians and families alike. Ultimately, while the promise of AI in pediatric oncology is compelling, careful navigation of these challenges is essential for successful implementation.
The Future of Pediatric Oncology with AI Innovations
The future of pediatric oncology looks increasingly bright with the innovations being driven by AI and machine learning tools. As researchers refine algorithms that can predict cancer relapse more effectively and accurately, the potential exists not only for improved survival rates but also for enhanced quality of life for young patients and their families. Continuous advancements in brain tumor imaging through AI will allow for more personalized treatment plans that consider individual patient histories and tumor behaviors.
Future clinical trials will likely focus on incorporating AI-driven predictions into standard operating procedures within pediatric oncology units, having the ability to shift care paradigms significantly. By tailoring the frequency of imaging and intervention based on AI predictions, clinicians can provide a higher resolution of care, ensuring that the most vulnerable patients receive the attention they need without unnecessary stress. The convergence of technology and healthcare promises to redefine pediatric cancer care in profound ways, paving the way for next-generation treatments.
Understanding Glioma Recurrence in Pediatric Patients
Gliomas in children comprise a spectrum of tumors with varying degrees of aggressiveness and treatment responses. Understanding glioma recurrence is crucial since it’s often a pivotal factor in determining treatment plans and prognoses. Traditional imaging techniques provide snapshots of a tumor’s status at a single point in time, leaving many gaps in knowledge about its progression. However, AI tools leveraging temporal learning offer insights that can indicate how a tumor may evolve and its likelihood of recurrence.
Incorporating temporal data into the analysis of pediatric gliomas allows for the monitoring of growth patterns and responses to treatment over time. This enhanced understanding not only informs clinicians about potential relapse risks but also supports families facing the uncertainties of their child’s disease. As healthcare evolves to embrace such advanced techniques in brain tumor imaging, the management of gliomas in pediatric patients will undoubtedly become more refined and effective.
The Importance of Early Detection in Pediatric Cancer
Early detection of pediatric cancer recurrence can dramatically improve treatment outcomes and survival rates. With the traditional reliance on clinical symptoms and occasional imaging, many recurrences are identified too late, limiting the effectiveness of subsequent treatment. AI-driven predictive models enhance the ability to catch these critical changes much sooner, particularly with technologies like temporal learning that analyze a patient’s imaging history over months.
By enabling earlier intervention, AI not only supports the clinical management of pediatric patients but fosters a proactive approach to care addressing the possibility of glioma relapse. Thus, it helps to shift the narrative from reactive to preventive care, benefiting patients and relieving the emotional turmoil endured by families faced with uncertainty about the future. As strides are made in AI cancer prediction, the role of early detection will continue to be pivotal in pediatric oncology.
Enhancing Imaging Practices for Children with Brain Tumors
Optimization of imaging practices is crucial in the care of children with brain tumors such as gliomas. The traditional methods may not only be time-consuming but may also subject young patients to unnecessary stress and exposure. AI-driven imaging techniques demonstrate the potential to streamline the process, allowing for more focused and insightful assessments based on data over time. AI cancer prediction technology can lead to a reduction in redundant imaging, paving the way for a more efficient workflow.
Continuous advancements in brain tumor imaging technology are promising for enhancing pediatric care. With models that analyze sequential scans, healthcare providers can understand tumor dynamics better and tailor follow-up protocols accordingly. This evolution in imaging practices not only expedites the diagnostic process but also equips clinicians with deeper insights into how to manage a child’s treatment journey proactively, marking a pivotal shift in the standard of care for pediatric oncology.
Collaboration and Research in Pediatric Oncology AI
The interdisciplinary approach to research in pediatric oncology AI has become increasingly essential. Collaborations among institutions like Mass General Brigham, Boston Children’s Hospital, and Dana-Farber Cancer Institute have demonstrated how pooling resources and expertise can enhance research outcomes. The combination of AI technology with clinical insights can significantly advance our understanding of childhood cancers such as gliomas and improve the predictive accuracy of relapse risk.
Ongoing research initiatives that focus on AI development and validation are crucial for establishing effective clinical practices based on these technologies. By working together, institutions play a vital role in bridging the gap between groundbreaking research and real-world applications. The commitment to collaborative efforts ensures that innovations like temporal learning AI continuously evolve, providing the best possible care for young patients facing the challenges of pediatric cancer.
Frequently Asked Questions
How does pediatric cancer relapse prediction differ from traditional methods?
Pediatric cancer relapse prediction using AI methods, particularly through temporal learning, surpasses traditional approaches by analyzing multiple brain scans over time. This allows for a more nuanced view of tumor behavior, especially in conditions like glioma, by recognizing subtle changes that single snapshot assessments might miss.
What role does AI cancer prediction play in assessing glioma recurrence?
AI cancer prediction plays a pivotal role in assessing glioma recurrence by utilizing advanced algorithms that evaluate multiple MRI scans. This method enhances the accuracy of predicting relapse risk in pediatric oncology patients, leading to timely interventions based on individual risk profiles.
Can temporal learning AI improve outcomes in pediatric oncology for brain tumors?
Yes, temporal learning AI can significantly improve outcomes in pediatric oncology, especially for brain tumors like gliomas, by providing accurate predictions on relapse. By analyzing sequences of MRI scans over time, this AI approach can help identify high-risk patients who may benefit from early intervention.
What is the importance of brain tumor imaging in pediatric cancer relapse prediction?
Brain tumor imaging, specifically through MRI, is crucial in pediatric cancer relapse prediction as it provides the necessary data for AI tools to analyze changes in tumor characteristics over time. This can lead to more informed decisions regarding treatment and monitoring plans in pediatric patients.
Why is early prediction of pediatric cancer relapse necessary?
Early prediction of pediatric cancer relapse is necessary to reduce the psychological and physical burden on young patients and their families. By identifying those at high risk, healthcare providers can tailor follow-up care and treatment strategies more effectively, leading to improved patient outcomes in pediatric oncology.
What findings support the efficacy of AI in pediatric cancer relapse prediction?
Recent findings indicate that an AI tool utilizing temporal learning has predicted cancer recurrence with an accuracy of 75-89% in pediatric patients, significantly outperforming traditional single-scan predictions, which had an accuracy of about 50%. This demonstrates the potential of AI in enhancing pediatric cancer care.
How can AI-informed predictions reduce imaging frequency for low-risk pediatric cancer patients?
AI-informed predictions can streamline the monitoring process; low-risk patients identified through accurate AI analysis may require fewer imaging sessions. This alleviates stress on children and families while maintaining effective oversight of potential relapse in pediatric cancer cases.
| Key Point | Details |
|---|---|
| New AI Tool | An AI tool predicts relapse risk in pediatric cancer more accurately than traditional methods. |
| Study Background | Conducted by researchers at Mass General Brigham and published in The New England Journal of Medicine AI, using data from 715 pediatric patients. |
| Temporal Learning Approach | This technique utilizes multiple brain scans over time to improve prediction accuracy. |
| Prediction Accuracy | The AI tool achieved 75-89% accuracy in predicting glioma recurrence one year post-treatment, compared to 50% accuracy with traditional single-image methods. |
| Future Prospects | Researchers aim to validate findings and explore clinical trials for AI-informed treatments. |
| Potential Benefits | This AI advancement might reduce frequent MR imaging for low-risk patients and offer targeted treatments for high-risk patients. |
Summary
Pediatric cancer relapse prediction is greatly enhanced by an innovative AI tool that outperforms traditional risk assessment methods. By analyzing multiple brain scans over time, this AI tool exhibits a significantly improved accuracy rate, which could transform the approach to monitoring and treating pediatric gliomas. With the potential to alleviate stress for families and optimize care by tailoring imaging frequency and treatment strategies, this research represents a significant leap forward in pediatric oncology.