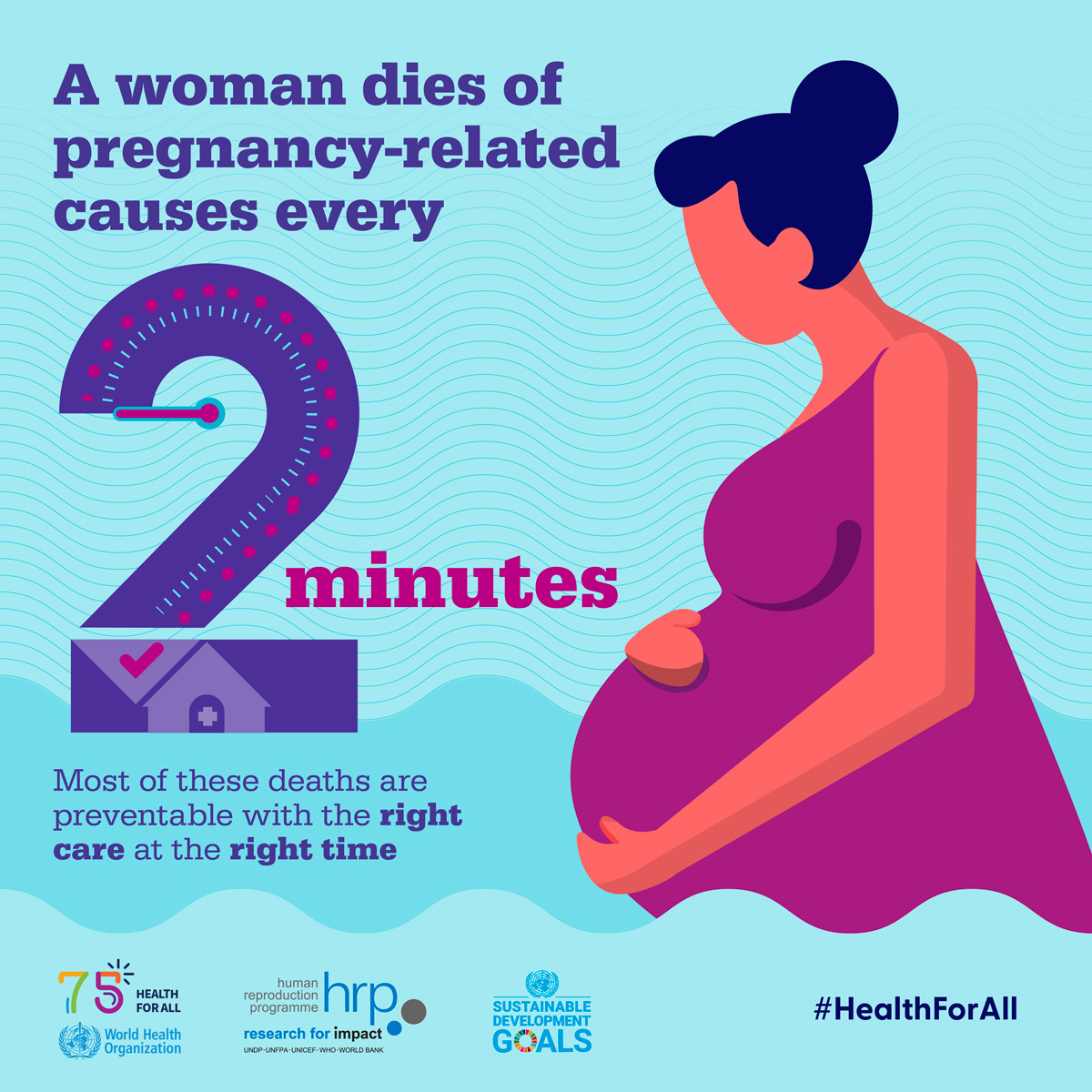
Maternal mortality is a pressing public health issue in the United States, underscoring a troubling trend in U.S. maternal health statistics. Despite advancements in medical care, the nation still leads among high-income countries in pregnancy-related deaths, which have shown alarming increases from 2018 to 2022. A staggering 80 percent of these deaths are preventable, calling for immediate attention to the postpartum care importance and the healthcare disparities that persist based on race and ethnicity. Racial disparities in maternal mortality rates highlight systemic inequalities, with American Indian and Alaska Native women facing significantly higher risks compared to their white counterparts. Addressing this crisis requires a multifaceted approach to combat preventable pregnancy deaths and enhance care for vulnerable populations.
The challenge of maternal mortality reflects broader concerns regarding women’s health during and after pregnancy. This term, often synonymous with pregnancy-related fatalities, encapsulates the unfortunate reality that many women face life-threatening complications during childbirth or the immediate postpartum period. Factors contributing to these tragic occurrences range from insufficient prenatal care to the significant influence of chronic health conditions. Improving maternal health outcomes necessitates recognizing the criticality of effective postpartum support and tackling the racial inequalities that have long marred our healthcare system. As we strive for progress, understanding maternal mortality through diverse lenses will ultimately guide us in designing strategies for better care and support for all mothers.
The Current State of U.S. Maternal Mortality Rates
As of 2023, the United States continues to grapple with alarmingly high maternal mortality rates, with a reported 32.6 deaths per 100,000 live births in 2022, a stark increase from 25.3 in 2018. This troubling trend has placed the U.S. at the forefront of maternal mortality rates among high-income countries, highlighting a systemic failure in prenatal and postpartum care. Factors contributing to this rise include chronic health conditions, socioeconomic disparities, and a fragmented healthcare system that often leaves vulnerable populations without adequate support.
Notably, over 80% of these pregnancy-related deaths are preventable, suggesting a dire need for intervention. Recent studies have indicated that the highest mortality rates are found among American Indian and Alaska Native women, who experience nearly four times the risk of their white counterparts. The intersection of race and policy demonstrates how deeply ingrained social inequalities contribute to disparities in maternal health, necessitating urgent reforms in healthcare accessibility and quality.
Understanding Racial Disparities in Maternal Health
Racial disparities in maternal mortality are stark and significant, revealing a troubling pattern where systemic inequities affect health outcomes for women of color. Data indicates that Black women face a mortality rate of 76.9 deaths per 100,000 live births, which is disproportionately high compared to white women. This continued inequity in maternal health underscores the urgent need for targeted policies that not only address healthcare access but also combat bias within the healthcare system.
Differences in clinical care, treatment access, and the social determinants of health all play pivotal roles in these disparities. Addressing the higher rates of preventable pregnancy deaths among marginalized groups involves multifaceted solutions, including cultural competency training for healthcare providers and community-based programs aimed at supporting women through pregnancy and postpartum care. Fostering an inclusive healthcare environment is crucial for reducing maternal mortality rates across racial and ethnic lines.
Enacting robust policies may bridge these gaps, ensuring equitable healthcare access to all pregnant individuals, particularly those historically marginalized.
The Role of Postpartum Care in Maternal Health
Postpartum care plays a critical role in preventing maternal mortality, especially given that nearly a third of maternal deaths occur between 42 days and one year after childbirth. Historically, U.S. healthcare systems have focused heavily on the immediate postpartum period, often neglecting the extended recovery phase that can significantly impact maternal health. As research indicates, complications related to cardiovascular diseases and mental health conditions can arise during this time, necessitating continuous medical support.
Improvement in postpartum care infrastructure can help mitigate preventable deaths by introducing comprehensive care plans tailored to individual needs. Investment in postpartum education programs that inform new mothers about warning signs, chronic conditions, and healthcare resources is essential. By embracing a holistic approach to maternal health that extends beyond the first six weeks postpartum, the U.S. can better address the factors contributing to maternal mortality.
Importance of Tracking Maternal Mortality
Effective tracking of maternal mortality is vital for understanding and addressing preventable pregnancy deaths. The implementation of a national system for recording maternal deaths in the U.S. did not fully commence until 2018, undermining previous efforts to adequately assess and improve maternal health outcomes. With the pregnancy checkbox on death certificates now fully in effect, researchers have begun to compile comprehensive data that can illuminate trends and inform policy decisions.
Accurate data allows for a better understanding of the factors contributing to maternal mortality rates, from chronic health issues to access to quality prenatal and postpartum care. This information is essential for policymakers aiming to implement strategic interventions directed at reducing deaths. By prioritizing data collection and analysis, stakeholders can identify gaps in healthcare delivery and create targeted initiatives designed to enhance maternal health systems.
Policy Recommendations for Reducing Maternal Mortality
To tackle the persistent issue of maternal mortality, comprehensive policy reforms are needed to improve care during pregnancy and the postpartum period. Recommendations include increasing funding for maternal health programs, enhancing healthcare workforce training, and expanding access to care in underserved communities. An emphasis should be placed on creating equitable healthcare policies that consider the unique challenges faced by different racial and ethnic groups.
Additionally, state-level policies must be scrutinized to understand disparities across regions, as the data indicates significant variations in maternal mortality rates. By adopting successful strategies from states that perform well, a framework can be established to improve outcomes nationwide. The investment in public health infrastructure is paramount to ensure sustainable improvements in maternal health and to curtail preventable pregnancy deaths.
The Impact of Chronic Conditions on Maternal Health
In recent years, a shift has been observed in the leading causes of maternal mortality, with chronic conditions such as cardiovascular disease now accounting for over 20% of pregnancy-related deaths. This trend is troubling, as younger individuals are increasingly presenting with chronic conditions that historically emerged later in life. Recognizing and managing these conditions before, during, and after pregnancy is crucial for reducing the associated risks.
Healthcare providers must increase awareness and screening for conditions like hypertension and diabetes among pregnant individuals, particularly for those at higher risk. This proactive approach can help tailor individualized care plans and potentially prevent severe outcomes. Addressing these underlying health issues is also critical in reducing the racial disparities seen in maternal mortality rates.
The Importance of Community-Based Interventions
Community-based interventions are essential for addressing the social determinants of health that contribute to maternal mortality. By empowering local organizations to provide support tailored to their communities’ unique needs, these initiatives can significantly impact the health outcomes for pregnant individuals. Programs could include prenatal education, mental health support, and access to transportation for medical appointments, all of which play critical roles in maternal survival.
Additionally, engaging communities in awareness campaigns can help disseminate information regarding the risks associated with pregnancy-related complications and the importance of seeking timely medical care. Collaborative efforts among healthcare providers, community leaders, and policymakers can foster environments where pregnant individuals feel supported and empowered to prioritize their health, ultimately working to reduce maternal mortality rates.
Addressing the COVID-19 Impact on Maternal Health
The COVID-19 pandemic has had a significant and lasting impact on maternal health, contributing to an increase in pregnancy-related deaths during and after the peak of the pandemic. As healthcare systems were stretched to their limits, many individuals faced barriers to accessing essential prenatal and postpartum care. This disruption has exposed the vulnerabilities within the U.S. healthcare system and the necessity for adaptable solutions.
As we move forward, understanding how the pandemic has redefined maternal health is crucial for implementing effective policies and practices. Prioritizing access to care during public health emergencies, developing telehealth solutions, and ensuring continuity of care for pregnant individuals is vital in mitigating the long-term consequences of COVID-19 on maternal mortality. The lessons learned must inform future preparedness strategies to ensure maternal health continues to be prioritized.
The Future of Maternal Health: A Call to Action
While significant challenges remain in the fight against maternal mortality in the United States, a concerted effort from all stakeholders can create a pathway toward improved outcomes. There is a pressing need for investment in maternal health infrastructure, policy reforms aimed at equity, and community-based initiatives that prioritize the voices of those most affected. It is crucial to integrate multidisciplinary approaches that involve healthcare providers, policymakers, and community leaders.
The future of maternal health depends on collaboration and innovation. As the medical community, policymakers, and advocates work together to build comprehensive care systems that address the needs of all pregnant individuals, the goal of reducing preventable pregnancy deaths could become an attainable reality. With proper commitment and resources, it is possible to transform the landscape of maternal health for the better.
Frequently Asked Questions
What are the current U.S. maternal health statistics regarding pregnancy-related deaths?
As of 2022, the U.S. maternal mortality rate is 32.6 deaths per 100,000 live births, marking a rise from 25.3 deaths per 100,000 live births in 2018. Significant disparities exist, with American Indian and Alaska Native women facing the highest mortality rate.
Why are pregnancy-related deaths considered preventable in the U.S.?
Over 80% of pregnancy-related deaths in the U.S. are classified as preventable. Key factors contributing to these deaths include inadequate prenatal care, systemic healthcare biases, and varying access to quality postpartum care, particularly among marginalized racial groups.
What role do racial disparities play in U.S. maternal mortality rates?
Racial disparities are stark in U.S. maternal mortality, with rates for American Indian and Alaska Native women at 106.3 deaths per 100,000 live births, nearly four times greater than those of white women. Systematic inequities contribute significantly to these differences.
How important is postpartum care in reducing maternal mortality?
Postpartum care is crucial in addressing maternal mortality, as nearly one-third of pregnancy-related deaths occur between 42 days and one year after birth. Comprehensive care during this period can identify and manage health issues that may arise post-pregnancy.
What health issues are most associated with maternal mortality in the U.S.?
Cardiovascular disease is the leading cause of pregnancy-related deaths in the U.S., accounting for over 20% of cases. Chronic conditions, especially hypertension, are increasingly affecting mothers, indicating a need for better management of these health issues.
What steps can be taken to improve U.S. maternal health outcomes?
Improving maternal health outcomes requires increased investment in public health infrastructure, enhanced access to quality prenatal and postpartum care, and addressing systemic disparities in healthcare systems across states.
Why should late maternal deaths matter in the discussion of maternal mortality?
Late maternal deaths, which occur from 42 days to one year postpartum, are significant as they highlight the need for comprehensive healthcare systems that extend past the immediate postpartum period, emphasizing the ongoing risk mothers face.
How can state-level variations in maternal mortality rates be addressed?
Addressing state-level variations requires targeted policy changes, greater investment in healthcare infrastructure, and the implementation of best practices from states that achieve lower maternal mortality rates.
What impact has the COVID-19 pandemic had on maternal mortality rates?
The COVID-19 pandemic has significantly influenced maternal mortality rates, especially in 2021, when an uptick was observed. This underscores the need for sustained focus on maternal healthcare even in times of crisis.
What data improvements have been made to track maternal mortality in the U.S.?
The implementation of the pregnancy checkbox on death certificates since 2018 has improved tracking of maternal mortality in the U.S., allowing for better data collection and analysis of pregnancy-related deaths.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality in the U.S. | The U.S. has the highest rate of maternal mortality among high-income countries, which increased from 25.3 in 2018 to 32.6 deaths per 100,000 live births in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable, indicating a significant opportunity for improvement. |
| Disparities in Maternal Mortality | There are significant disparities by state, race, and ethnicity; American Indian women have the highest mortality rate. |
| Leading Causes of Pregnancy-Related Death | Cardiovascular diseases are now the leading cause of maternal death, accounting for over 20% of cases. |
| Importance of Late Maternal Deaths | Late maternal deaths, which occur within a year of pregnancy, account for nearly one-third of total deaths and are increasingly recognized. |
| Public Health Infrastructure Needs | There is a critical need for improved public health infrastructure and investment in maternal health care systems to reduce mortality rates. |
Summary
Maternal mortality is a critical issue that continues to affect thousands in the U.S. Despite advancements in healthcare, the country has maintained the highest maternal mortality rate among high-income nations. Addressing preventable deaths through enhanced prenatal care and better postpartum support is essential. Moreover, recognizing and acting upon the significant disparities faced by minority groups can help create a more equitable healthcare system. Continuous investment in public health infrastructure is vital to ensure that every mother has access to quality care, thus reducing maternal mortality rates in the future.