AI predicting brain cancer relapse represents a groundbreaking advancement in pediatric oncology, particularly in managing cases of glioma. A recent study conducted by researchers at Mass General Brigham demonstrated that an AI tool could analyze multiple brain scans over time, achieving significantly higher accuracy in predicting cancer recurrence compared to traditional methods. This improved brain cancer prediction could alleviate stress for young patients and their families, who often endure years of frequent follow-ups and imaging to monitor recurrence risk. By employing innovative techniques like temporal learning in medicine, the researchers have set the stage for AI in cancer treatment to transform how healthcare professionals approach pediatric gliomas. As more data becomes available, the potential for this technology to enhance patient care continues to grow, promising to provide personalized treatment plans based on individual recurrence risks in pediatric cancer cases.
Artificial Intelligence (AI) and its role in forecasting brain cancer relapses are revolutionizing the landscape of pediatric cancer care. An innovative study by the team at Mass General Brigham showcased an AI application that predicts the reappearance of brain tumors, particularly gliomas, with remarkable precision. This method not only surpasses the reliability of conventional prediction techniques but also signifies a shift towards using advanced analytics in understanding recurrence patterns. Leveraging concepts such as temporal learning, which involves analyzing sequences of images over time, offers new insights into managing the risks associated with pediatric brain cancers. As this technology evolves, it exemplifies a future where individualized treatment strategies can be designed, significantly improving outcomes for young cancer patients.
The Role of AI in Pediatric Glioma Management
Artificial intelligence (AI) is revolutionizing how pediatric gliomas, a type of brain tumor, are managed in clinical settings. This advancement stems from the integration of complex algorithms that can not only identify the presence of tumors but also offer predictions regarding their growth and potential relapse. By analyzing thousands of MRI scans over time, these AI tools provide insights that were previously obscured, allowing for personalized treatment plans tailored to individual patient risks. This innovative approach aims to bridge the gap between traditional methods and more precise predictive analytics, ultimately improving patient outcomes in pediatric cancer care.
The predictive capabilities of AI extend to assessing the likelihood of recurrence in pediatric glioma cases, which is a significant concern for both families and healthcare professionals. Conventional follow-up assessments often require frequent imaging, causing stress and anxiety among young patients. However, by utilizing machine learning techniques—specifically temporal learning—AI can gauge the recurrence risk more accurately, potentially reducing the number of unnecessary scans for low-risk patients. This not only alleviates some of the emotional and logistical burdens on families but also allows healthcare providers to focus their resources on high-risk individuals who may benefit from more aggressive follow-up or treatment.
AI Predicting Brain Cancer Relapse: A Paradigm Shift
Recent studies highlight the remarkable ability of AI systems to predict brain cancer relapse, particularly in pediatric populations. By leveraging temporal learning, researchers have demonstrated that AI can accurately analyze sequential MRI scans over time, leading to predictions of recurrence that surpass the capabilities of traditional diagnostic methods. This methodological shift indicates that AI tools are not just adjuncts to existing technology; they are rapidly becoming central to the process of managing brain tumor recurrence risks in children, facilitating a proactive rather than reactive approach to treatment.
The implications of AI predicting brain cancer relapse extend beyond mere predictions; they signify a transformation in how treatment paradigms are constructed. By foreseeing potential recurrence, healthcare providers can implement early interventions tailored to each patient’s unique risk profile. For instance, preventive therapies can be administered ahead of time, minimizing the chances of complications and enhancing overall treatment efficacy. As more data becomes available and AI models improve, the hope is to not only optimize individual patient care but also advance the collective knowledge regarding brain cancer recurrence in pediatric populations.
Temporal Learning in Medicine: Enhancing Prediction Accuracy
Temporal learning represents a groundbreaking technique in the medical AI landscape, particularly in the prediction of disease progression. By analyzing multiple imaging modalities and their sequence, temporal learning enables AI models to identify trends and subtle changes that may indicate a shift in a patient’s condition over time. This methodology is particularly advantageous in the context of pediatric gliomas, where timing is critical, and the stakes are high. With the ability to collate and evaluate data from several MR scans—as opposed to relying on a singular snapshot—this technique enhances the precision of recurrence predictions.
The successful implementation of temporal learning in predicting outcomes for pediatric glioma patients showcases its potential applicability across various medical fields. By improving the accuracy of predictions, medical professionals can make more informed decisions and tailor interventions based on a patient’s specific trajectory. As more healthcare settings adopt such technologies, the insights gained could yield broader implications for managing recurrence risk in pediatric cancer and even other diseases, ushering in a new era of personalized medicine guided by data-driven intelligence.
Challenges and Future Directions in AI for Cancer Treatment
Despite the promising advancements in AI for predicting cancer recurrence in pediatric patients, several challenges remain. One significant hurdle is ensuring the accuracy and reliability of AI predictions across diverse patient populations and clinical settings. As the research progresses, continued validation is crucial to support the transition from clinical trials to everyday practice. Researchers must also address the interpretability of AI outcomes, as understanding the ‘why’ behind predictions is essential for clinician trust and patient acceptance.
Looking ahead, the future of AI in cancer treatment could be transformative. Researchers envision a world where AI not only predicts relapse but also informs treatment decisions actively. By integrating real-time data from patient monitoring and imaging, AI could facilitate dynamic treatment plans that adapt to a patient’s evolving condition. As this technology develops, ensuring ethical considerations and data privacy will also be paramount, helping to harness AI’s full potential while safeguarding patient rights.
Integrating AI Insights into Pediatric Cancer Care
Integrating AI insights into pediatric cancer care stands to significantly enhance the effectiveness of treatment protocols for brain tumors. This encompasses not only the prediction of recurrence but also the timing and type of interventions that may be necessary post-surgery. As hospitals begin to adopt AI tools, the focus will shift periodically from reactive measures to proactive strategies, where children can receive interventions based on AI-derived risk assessments, ultimately improving their quality of life and health outcomes.
Moreover, the collaborative effort among institutions—such as those seen in recent studies—highlights the importance of shared knowledge and resources in cancer research. By pooling data and insights, hospitals can refine AI algorithms and create a more comprehensive understanding of pediatric brain cancer. This move towards a collaborative model will ensure that advancements in AI are disseminated widely, making state-of-the-art predictive tools accessible for all patients in need.
The Future of Pediatric Cancer Prediction with AI Technology
The future of pediatric cancer prediction seems bright with the advent of AI technologies that are tailored to detect relapses in brain tumors like gliomas. As researchers continue to refine these predictive models, there exists an immense opportunity to dramatically improve survival rates amongst children diagnosed with cancer. Implementing more advanced AI-driven techniques will not only aid in predicting recurrence but also in personalizing treatment plans that could ultimately enhance patient outcomes.
As AI continues to evolve, embracing advanced data analysis techniques could lead to breakthroughs in understanding malignancies. Moreover, developing partnerships between machine learning researchers and medical professionals will prove essential in pushing the boundaries of current capabilities. The goal is to create a comprehensive system that ensures all pediatric cancer patients can benefit from tailored interventions, reducing the burden of disease and improving their overall health trajectories.
Challenges of Recurrence Risk Assessment in Pediatric Gliomas
Assessing recurrence risk in pediatric gliomas presents unique challenges due to the complex nature of brain tumors in children. Each tumor presents a unique profile and responds differently to treatment, which complicates the establishment of standardized predictive models. Additionally, the variations in individual patient responses to surgical procedures, coupled with their diverse genetic and environmental backgrounds, necessitate a more personalized approach to risk assessment.
Current models, while effective to an extent, still rely heavily on historical data, which may not fully encapsulate the nuances of new treatment modalities or the evolving landscape of pediatric oncology. Advancements in AI and machine learning provide an avenue to refine these predictive measures, but thorough validation across diverse clinical scenarios is paramount before any widespread adoption of these techniques can occur.
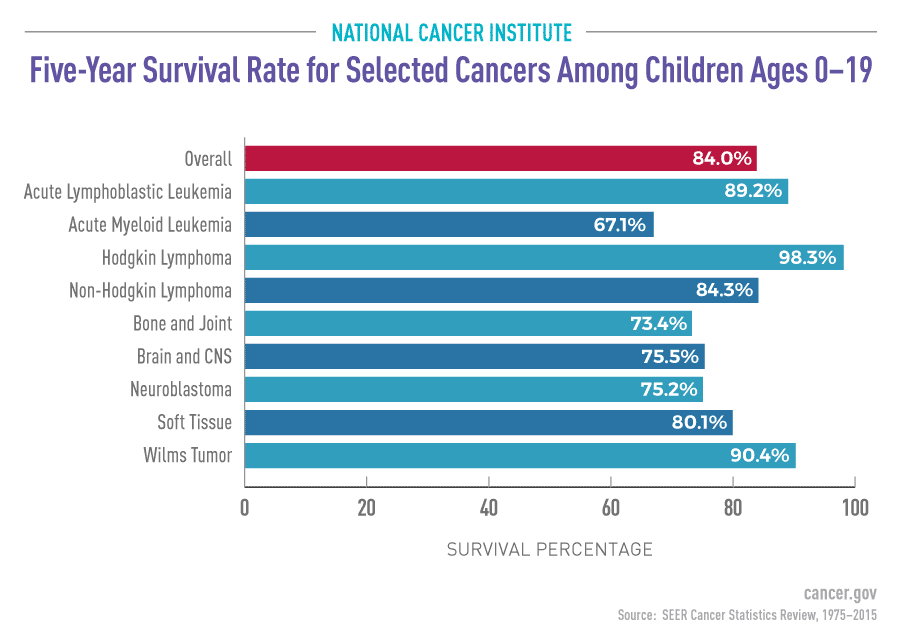
The Importance of Early Detection in Pediatric Cancer Treatment
Early detection of pediatric cancers, including brain tumors like gliomas, is critical for improving survival rates and treatment outcomes. The ability to predict recurrence risks accurately can lead to timely intervention and significantly impact patient prognosis. Employing advanced AI tools can facilitate this early detection, enabling healthcare providers to identify at-risk patients and customize their treatment plans accordingly, thus supporting better outcomes in this vulnerable population.
Furthermore, the emphasis on early detection extends beyond initial diagnosis; it encompasses ongoing monitoring to ensure that patients remain free of disease. As the research advances in utilizing AI for continuous assessment, it provides a promising frontier in pediatric oncology. By harnessing the power of technology to catch signs of recurrence early, children can receive the best possible care, minimizing the impact of potential relapses.
Future Directions in AI for Personalized Medicine
The future of personalized medicine, particularly in pediatric oncology, hinges on the successful integration of AI technologies. These advancements promise to tailor treatment approaches to individual patient profiles, enhancing the precision with which care is delivered. With AI’s capacity to analyze immense datasets, treating clinicians can receive actionable insights regarding recurrence risk, treatment responses, and necessary adjustments—all designed to align with the unique circumstances of each young patient.
As researchers continue to explore the intersection of AI and personalized medicine, ongoing education for healthcare professionals will be essential to ensure these tools are used effectively and responsibly. The implementation of AI-driven predictive models in clinical practices represents a significant leap towards individualized care, which is crucial in enhancing the treatment success rates in pediatric glioma and other childhood cancers.
Frequently Asked Questions
How is AI used in predicting brain cancer relapse in pediatric glioma patients?
AI is utilized in predicting brain cancer relapse by analyzing longitudinal brain scans taken over time. A recent study indicates that an AI tool, leveraging temporal learning, provides more accurate predictions about recurrence in pediatric glioma patients compared to traditional methods. Instead of relying on single imaging snapshots, the AI synthesizes findings from multiple scans, improving its ability to detect subtle changes that indicate a risk of relapse.
What are the benefits of using AI in brain cancer prediction for children?
The benefits of using AI in brain cancer prediction for children, especially those with pediatric glioma, include enhanced accuracy in determining recurrence risk, reducing the need for frequent and stressful imaging tests. The AI’s ability to identify high-risk patients early allows for better management of care, potentially leading to timely interventions and less emotional and physical burden on patients and their families.
What is temporal learning in medicine and how does it help in brain cancer prediction?
Temporal learning in medicine refers to a technique where AI models learn from sequences of data collected over time. In the context of brain cancer prediction, this approach allows the AI to analyze multiple MRI scans of patients post-surgery, recognizing patterns and changes that indicate the likelihood of cancer relapse. This method has significantly improved accuracy in predicting recurrence risk in pediatric glioma.
What are the implications of improved AI in cancer treatment for pediatric glioma patients?
Improved AI in cancer treatment can lead to significant advancements for pediatric glioma patients by providing more reliable predictions of relapse, which can inform personalized treatment strategies. This may reduce unnecessary imaging for lower-risk patients and facilitate proactive measures, like targeted therapies, for those at higher risk of recurrence, ultimately enhancing patient outcomes and quality of life.
What is the accuracy of AI predictions for relapse risk in pediatric brain cancer?
The AI tool developed for predicting relapse risk in pediatric brain cancer patients demonstrated an accuracy rate of 75-89% for identifying recurrence of gliomas one year post-treatment. This level of precision is notably higher than traditional methods, which only achieved approximately 50% accuracy based on single image analyses.
What further steps are needed before implementing AI in clinical settings for brain cancer prediction?
Before implementing AI in clinical settings for brain cancer prediction, further validation of the technology across diverse patient populations and settings is essential. Researchers aim to conduct clinical trials to assess whether AI-informed predictions indeed lead to improved care practices, such as adjusted imaging frequency and preemptive therapies for high-risk pediatric glioma patients.
How might AI reduce the burden of medical imaging for pediatric cancer patients?
AI has the potential to reduce the burden of medical imaging for pediatric cancer patients by accurately identifying those at low risk of relapse. This could lead to fewer follow-up imaging sessions, alleviating stress and anxiety for both children and their families, while ensuring that high-risk patients receive the necessary monitoring and treatment.
What role do MRI scans play in AI predictions of brain cancer relapse?
MRI scans play a crucial role in AI predictions of brain cancer relapse by providing the raw imaging data that the AI analyzes. By examining multiple scans over time, the AI application can detect nuanced changes that signify the risk of recurrence in pediatric glioma patients, thus making far more accurate predictions than those based on isolated scans.
| Key Point | Details |
|---|---|
| AI Predicting Relapse Risk | An AI tool can better predict the risk of relapse in pediatric brain cancer patients compared to traditional methods. |
| Study Background | The study was conducted by researchers at Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, and analyzed nearly 4,000 MR scans from 715 pediatric patients. |
| Temporal Learning Method | This novel technique involved training the AI model using multiple scans taken over time, allowing better recognition of subtle changes in the patient’s condition. |
| Prediction Accuracy | The AI model predicted recurrence of glioma within one year post-treatment with 75-89% accuracy, significantly higher than the 50% accuracy of traditional methods. |
| Clinical Implications | Further validation is needed, but the researchers aim to use AI predictions to improve patient care and potentially reduce unnecessary imaging. |
Summary
AI predicting brain cancer relapse has shown significant promise in improving patient outcomes. By utilizing advanced AI tools that analyze brain scans over time, researchers have developed a method that predicts relapse risk in pediatric glioma patients with much greater accuracy than existing traditional techniques. This innovation not only has the potential to enhance the quality of care provided to young cancer patients but also aims to alleviate the stress associated with frequent imaging by identifying those at the highest risk for recurrence. Continued research and validation will be crucial in realizing the full benefits of this approach for clinical applications.