Alzheimer’s disease research has made significant strides in recent years, reshaping our understanding of the brain’s immune system and its role in neurodegenerative diseases. Leading this transformative effort is neuroscientist Beth Stevens, whose groundbreaking studies focus on microglial cells—the brain’s defenders against illness and injury. These cells are vital for maintaining a healthy brain environment, but their pruning of neuronal connections can sometimes go awry, potentially contributing to the onset of Alzheimer’s. With generous support from NIH funding, Stevens and her team are uncovering new paths for innovative therapies and biomarkers that could revolutionize Alzheimer’s diagnosis and treatment. Given that millions of Americans are currently affected, her work is not only relevant but essential in combating this growing public health crisis.
Explorations into Alzheimer’s have opened new avenues for understanding various forms of cognitive decline and memory impairment. Intersecting with fields such as immunology and neurobiology, the study of how microglial cells interact with neurons has garnered attention as a critical area of study. Researchers like Beth Stevens are at the forefront, leveraging insights into the brain’s immune mechanisms to combat disorders associated with aging. By harnessing federal support and focusing on the cellular processes involved in synaptic pruning, they aim to develop novel interventions that address the challenges posed by Alzheimer’s and related diseases. This holistic approach not only promises to improve current therapeutic strategies but also paves the way for early detection and enhanced patient outcomes.
Understanding Microglial Cells in Alzheimer’s Research
Microglial cells, often referred to as the brain’s immune system, play a crucial role in maintaining neurological health. In the context of Alzheimer’s disease, their functions are particularly significant as they help clear away debris from dead or damaged neurons. Research led by scientists like Beth Stevens highlights that when these cells malfunction, they may inadvertently contribute to the progression of neurodegenerative diseases. By better understanding how microgliosis—an inflammatory response by microglial cells—occurs, researchers can unlock new therapeutic avenues for combating Alzheimer’s and related disorders.
Moreover, studies on microglial cells have revealed their dual role in synaptic pruning, which is essential in normal brain function. However, this pruning process can sometimes go awry, leading to synaptic loss and cognitive decline, hallmark characteristics of Alzheimer’s disease. The work being done in Stevens’ lab not only focuses on the traditional pathways of microglial activity but also seeks to discover how alterations in these processes can predict and identify neurodegenerative conditions earlier than current methods allow.
The Role of NIH Funding in Advancing Alzheimer’s Research
Federal funding, particularly from the National Institutes of Health (NIH), has been instrumental in propelling Alzheimer’s disease research forward. For researchers like Beth Stevens, NIH grants provide vital resources necessary for exploring innovative ideas that link microglial dysfunction to neurodegenerative diseases. Such funding ensures that promising lines of inquiry can be pursued in-depth, enabling scientists to investigate complex mechanisms that govern immune response in the brain. Stevens emphasizes that this support is foundational, allowing her lab to transition from basic science to discovering practical solutions that may lead to alleviating symptoms of Alzheimer’s.
Additionally, maintaining consistent NIH funding allows for sustained research efforts, which is especially crucial in fields like neurobiology where discoveries can take years, if not decades, to materialize into tangible benefits. The continuity afforded by these grants fosters a fertile ground for scientific exploration and collaboration, ultimately leading to breakthroughs that could improve the lives of millions suffering from Alzheimer’s and other neurodegenerative diseases. As researchers continue to follow the threads laid down by the early explorations of microglial function, the impact of NIH funding cannot be overstated in its role as a catalyst for scientific advancement.
Innovations in Neurodegenerative Disease Treatment
Research into neurodegenerative diseases has evolved dramatically, with a particular focus on uncovering new treatment modalities. One exciting development comes from understanding the critical role of microglial cells in diseases such as Alzheimer’s and Huntington’s disease. By leveraging insights gained from studies conducted in labs like that of Beth Stevens, researchers are identifying novel pathways that could be targeted with new pharmaceuticals. These innovations not only aim to halt disease progression but also strive to restore cognitive functions that are often lost as a result of these conditions.
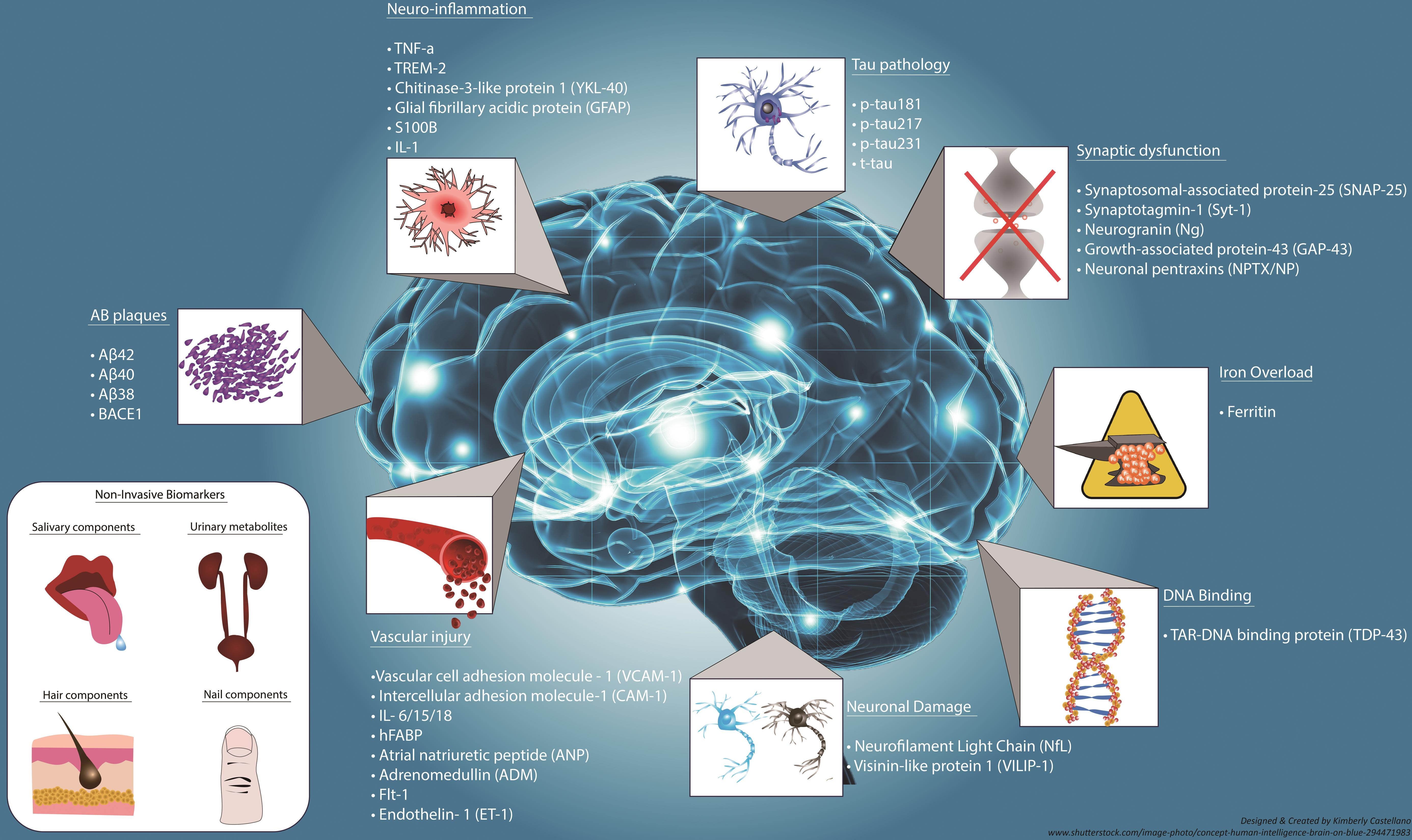
Furthermore, the integration of findings from diverse fields—ranging from neuroimmunology to molecular biology—illustrates the potential for interdisciplinary approaches to yield innovative therapies. As new biomarkers are discovered for early diagnosis, there is a promising horizon for tailored treatments that are more effective and minimally invasive. Such advancements reflect a shift from traditional methodologies to a more comprehensive understanding of how various biological systems interact in the context of neurodegenerative diseases, paving the way for a future where conditions like Alzheimer’s can be tackled with precision medicine.
The Future of Alzheimer’s Research: A Holistic Approach
As the landscape of Alzheimer’s disease research continues to evolve, there is a significant shift towards adopting a holistic view of the brain’s immune system and its implications for neurodegenerative diseases. Scientists, including those in Beth Stevens’ lab, are now prioritizing a multi-faceted approach that examines how genetic, environmental, and cellular factors contribute to the onset and progression of Alzheimer’s. This comprehensive strategy not only enhances our understanding of the disease itself but also facilitates the identification of intervention points that can be targeted by future therapies.
In this new era of research, the insights gained from studying microglial cells are crucial. They offer clues about how the brain can repair itself after injury or disease and what happens when these processes fail. The ultimate goal is to create interventions that can not only stop Alzheimer’s in its tracks but also enable recovery of lost functions. By fostering collaboration among geneticists, neurobiologists, and clinicians, the potential for breakthroughs that will enhance the quality of life for millions continues to grow, underscoring the importance of sustained research efforts supported by institutions like the NIH.
Challenges in Alzheimer’s Disease Research
Despite the promising developments in Alzheimer’s disease research, significant challenges remain. The complexity of neurodegenerative diseases makes them particularly hard to study and treat. Factors such as the heterogeneous nature of Alzheimer’s, the variability in patient responses to treatments, and the ethical considerations of conducting research on human subjects all complicate the research landscape. Furthermore, the process of converting basic science discoveries about microglial dysfunction into effective clinical applications is fraught with obstacles.
Researchers, including Beth Stevens, advocate for continued investment in neuroscience research to overcome these barriers. An emphasis on long-term studies and interdisciplinary collaboration is essential to address the multifactorial nature of Alzheimer’s. With ongoing efforts to properly identify how immune responses in the brain can be harnessed for therapeutic benefits, the path forward is filled with both hurdles and opportunities. Building a robust framework for research will ultimately lead to a better understanding of Alzheimer’s pathology and the development of effective treatments.
The Importance of Early Detection in Alzheimer’s Disease
Early detection of Alzheimer’s disease is increasingly recognized as vital for improving patient outcomes. Advances in research, particularly in identifying biomarkers through the study of microglial cells, are paving the way for earlier and more accurate diagnoses. Detecting Alzheimer’s in its nascent stages allows for the implementation of interventions that may slow the progression of the disease, improve cognitive function, and enhance the quality of life for those affected. Beth Stevens’ work on microglial-related mechanisms has profound implications for how we approach early diagnosis and treatment.
Moreover, early detection can significantly reduce the healthcare burden associated with advanced stages of Alzheimer’s. As the population ages, understanding the importance of recognizing initial symptoms will help prepare healthcare systems and families for the challenges ahead. Research that focuses on early intervention strategies can lead to decreased care costs, improved patient outcomes, and greater quality of life for millions. The promise of early diagnosis is an exciting prospect in the fight against Alzheimer’s disease, reinforced by the scientific strides made in understanding the role of the brain’s immune system.
The Impact of Public Awareness on Alzheimer’s Research Funding
Public awareness of Alzheimer’s disease and its impact on individuals and families is crucial for driving funding and support for research initiatives. Greater understanding of the disease can lead to increased advocacy for resources allocated to critical studies, including those focusing on microglial cells as a therapeutic target. Prominent figures like Beth Stevens are working to increase visibility around the importance of the brain’s immune system in neurodegenerative disease research, underlining the need for sustained investment from both government and private sectors.
As communities become more educated about Alzheimer’s, this can translate into increased fundraising for research projects and support for policy initiatives that favor scientific inquiry. Engaging the public in conversations about the science behind Alzheimer’s disease helps demystify the complexities involved and fosters a culture of support for innovative research. By highlighting how foundational work in labs is unlocking new possibilities, advocates can galvanize community action that translates into tangible benefits for researchers and patients alike.
Collaboration: Key to Future Discoveries in Alzheimer’s Research
Collaboration across disciplines is emerging as a cornerstone of effective Alzheimer’s research. The increasingly complex nature of neurodegenerative diseases requires insights from various fields—including genetics, immunology, and neuroscience. Beth Stevens emphasizes that collaborative efforts have the potential to expedite discoveries related to microglial activity and its role in diseases like Alzheimer’s. By fostering relationships among researchers from different backgrounds, scientists can share knowledge and techniques that enhance their understanding of how neuroimmune interactions influence disease progression.
This collaborative spirit is also echoed in the way federal and private funding sources support joint projects that aim to tackle Alzheimer’s from multiple angles. Combining expertise from researchers who specialize in the brain’s immune system, molecular pathways, and clinical applications can lead to breakthroughs that are more impactful than isolated studies. As researchers continue to unite in the pursuit of understanding and treating Alzheimer’s disease, the potential for shared findings to lead to innovative solutions grows exponentially.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells serve as the brain’s immune system and are pivotal in Alzheimer’s disease research. They patrol the brain for illness and injury, clearing away dead cells and pruning synapses. Research indicates that improper pruning by microglia may contribute to neurodegenerative diseases like Alzheimer’s, emphasizing their importance in understanding and potentially treating the condition.
How has Beth Stevens contributed to Alzheimer’s disease research?
Beth Stevens has made significant contributions to Alzheimer’s disease research by transforming our understanding of microglial cells. Her lab’s findings show how these immune cells, when malfunctioning, can lead to issues in synaptic pruning, contributing to neurodegenerative diseases including Alzheimer’s. Her research lays the groundwork for new medications and diagnostic biomarkers.
What is the significance of NIH funding in Alzheimer’s disease research?
NIH funding is crucial for advancing Alzheimer’s disease research, as highlighted by scientists like Beth Stevens. This federal support has historically provided the foundation for innovative studies on microglial cells and their role in neurodegenerative diseases, enabling researchers to explore complex biological questions that could lead to new treatments and understandings of Alzheimer’s.
How can understanding the brain’s immune system aid Alzheimer’s disease research?
Understanding the brain’s immune system, particularly through the study of microglial cells, is essential in Alzheimer’s disease research. Insights into how these cells respond to cellular damage and their role in neuronal health can reveal mechanisms that contribute to Alzheimer’s, guiding the development of targeted therapies and interventions for affected patients.
What advancements in Alzheimer’s disease treatment are expected from ongoing research on microglial cells?
Ongoing research on microglial cells is expected to lead to advancements in Alzheimer’s disease treatment. By identifying how microglia contribute to synaptic dysfunction and neurodegeneration, scientists aim to create new medications that can enhance brain resilience and potentially reverse symptoms in patients, ultimately aiming to improve quality of life for millions living with Alzheimer’s.
| Key Points | Details |
|---|---|
| Researcher | Beth Stevens, neuroscientist at Harvard. |
| Research Focus | Microglial cells and their role in brain immunity. |
| Importance of Research | Improper microglial pruning linked to Alzheimer’s and other neurodegenerative diseases. |
| Potential Impact | Foundation for new Alzheimer’s disease medications and early detection biomarkers. |
| Future Estimates | Projected doubling of Alzheimer’s cases in the U.S. by 2050. |
Summary
Alzheimer’s disease research is increasingly vital as we uncover the fundamental role of microglial cells in the brain’s immune response, which directly impacts the understanding and treatment of Alzheimer’s disease. Neuroscientist Beth Stevens has highlighted how incorrect synaptic pruning by these immune cells can lead to neurodegenerative disorders, paving the way for innovative treatments. As the aging population grows, effective research and new discoveries will be crucial in managing the imminent rise in Alzheimer’s cases and their associated healthcare costs. Recognizing the significance of foundational science is essential for driving forward progress in Alzheimer’s research.